Current food production practices
The food we eat and the manner in which it is produced affect human health and impact the environment. Global meat production has changed over the last 100 years from primarily small-scale, diversified farms to a large, vertical system controlled by a small number of large corporations( Reference Graham, Leibler and Price 1 ). Meat and poultry production is particularly harmful to the environment because a majority is produced through industrial food animal production( Reference Silbergeld, Graham and Price 2 ). This system is able to keep the cost of food deceptively low through cheap inputs of water, energy, fossil fuel and primarily through government-subsidized grain for feed( Reference Gurian-Sherman 3 ). Although this type of production system works well to produce certain commodities cheaply in the short term, a mechanized approach to producing food fails to account for the hidden costs to the environment and human health in the low purchase price of meat( Reference Graham, Leibler and Price 1 , Reference Walker, Rhubart-Berg and McKenzie 4 ).
Environmental effects
These methods of producing meat have resulted in new environmental pathways for human and animal exposure to pathogenic bacteria through transfer from animal to environment to man and back( Reference Graham, Leibler and Price 1 ). The industrial agriculture model is a significant contributor to climate change. The FAO found that the animal agriculture sector emits 18 % of human-induced greenhouse gas emissions, which is greater than what is found in the US transportation sector( Reference Steinfeld, Gerber and Wassenaar 5 ). However, the major contributing source of greenhouse gas emissions is controversial and there are not sufficient tools to measure the global impact from the agricultural sector( Reference Tubiello, Salvatore and Rossi 6 ).
In addition to contributing greenhouse gas emissions, the industrial agriculture model is also associated with polluted air and groundwater through the collection, storage and spread of animal waste. In the USA, these facilities produce over 2·9 billion tonnes (1·3 billion tons) of manure annually; a figure 100 times greater than the amount of human sewage processed in US municipal wastewater plants every year( Reference Gerba and Smith 7 ).
Human health effects
Producing meat through an industrial system also has a deleterious impact on human health. Consumption of meat has increased steadily over time, especially in low- to middle-income countries, despite the increased risk of diseases like obesity, CVD and some forms of cancer( Reference McMichael, Powles and Butler 8 ). Of primary concern is the use of sub-therapeutic doses of antibiotics in food animals. Since World War II, the US Food and Drug Administration has allowed producers to give human medications to food animals at low doses to promote growth and prevent illness( 9 ). In fact, a 1995 report by the US Congressional Office of Technology Assessment estimated that close to 90 % of all antibiotics used during animal husbandry are as growth promoters or for disease prevention rather than for treatment of sick animals( 9 ). More recent estimates based on a report by the Food and Drug Administration suggest that this number is lower; although widely publicized in media outlets, the exact number has not been published( 10 ).
The use of these antibiotics in food animals can lead to resistant strains of bacteria, which threatens the efficacy of these medicines for people. In addition, as much as 75 % of antibiotics pass unchanged from feed to manure and create risks to soil and water quality( Reference Chee-Sanford, Aminov and Krapac 11 , Reference Kemper 12 ). Of additional concern are recent studies that have identified various controversial chemicals and additives in animal feed and subsequently in animal waste. These include arsenic, growth hormones, poultry litter, animal feathers and carcasses, caffeine and prescription drugs( Reference Walker, Rhubart-Berg and McKenzie 4 , Reference Love, Halden and Davis 13 ). Currently, there are no policies to ban the use of antibiotics in animal feed. Recent resolutions to end these practices have been made by the American Medical Association, the American Public Health Association, the American Nursing Association and recently by the Food and Drug Administration, to voluntarily restrict the use of sub-therapeutic doses of antibiotics for growth promotion, encourage healthier food systems and promote environmental sustainability within their organizations( 14 – 17 ).
Impact on the health-care system
Health-care organizations are uniquely poised to change the food system because they model health behaviours, possess incredible purchasing power and provide food to a large number of people every day. In the FoodService Director 2013 hospital census, hospitals located in the Northeast US region served meals to an average of 344 patients and 1974 visitors and staff daily( 18 ). In Maryland, hospitals employ nearly 100 000 workers making health care one of the largest private-sector employers( 19 ).
There is a growing consensus among the medical community to address the food environment within hospitals and health-care organizations. To date 489 hospitals, health systems and food service contractors in the USA have signed a Healthy Food Pledge, developed by the international non-profit coalition Health Care Without Harm (HCWH), dedicated to improve the health of their patients, communities and the environment( 20 ). However, each hospital may have unique needs, barriers to change, limited resources and facility or environmental challenges to overcome to implement a change to their food system.
Implementation of a healthy food programme
One initiative to address change and overcome barriers to improving the food environment of health care is the Balanced Menus Challenge (BMC). This programme is both a climate change mitigation strategy and an effort to bring the healthiest, most sustainably produced meat available into health-care settings to preserve antibiotic effectiveness and promote good nutrition.
The BMC addresses a major obstacle to changing the hospital food environment because purchasing meat is expensive. Outside labour costs, the largest expenditure for a typical hospital’s food service budget is the meat and poultry purchases( 19 ). Implementation of the BMC has demonstrated savings of the order of $US 20 000 annually for an average-sized hospital in the USA( Reference Lagasse and Neff 21 ).
Overview of the Balanced Menus Challenge
The BMC was developed in 2008 through two non-profit organizations: (i) HCWH and (ii) the non-profit educational organization, San Francisco Physicians for Social Responsibility( 20 – 22 ). The BMC is a voluntary commitment by health-care institutions to reduce their overall meat procurement within 12 months. The BMC is a two-tier programme whereby hospitals (i) reduce meat purchases by 20 % and then (ii) invest the cost savings into purchasing locally produced meat and/or meat with a smaller environmental footprint (Table 1).
Table 1 Balanced Menus Challenge strategy
The rationale of the programme is to reduce the overall amount of meat that is procured and served, thereby leading to a lower dollar:meal ratio. The money saved per meal can then be used to substitute more locally produced meat and/or meat with a smaller environmental footprint, which are typically more expensive than conventionally produced meat.
Balanced Menus Challenge: key definitions
-
1. In the BMC, ‘meat’ is broadly defined as beef, pork, lamb, bison, chicken, turkey, other poultry products, seafood and lunchmeats.
-
2. ‘Local foods’ are defined as those grown, raised and processed within 400 km (250 miles) of the health-care facility.
-
3. ‘Sustainable foods’ are defined as third-party certified and/or approved to carry one or more of the following label claims endorsed by the US Department of Agriculture or the Food and Drug Administration: ‘raised without antibiotics’, ‘no antibiotics administered’, ‘raised without added hormones’, ‘no hormones added’, ‘no genetically engineered ingredients’, ‘rBGH-free’, ‘rBST-free’ or ‘grass-fed’.
-
4. ‘Food service professional’ is defined as any person who is responsible for the procurement, design, delivery, preparation or tracking of food and meal service within the facility. Examples of titles held by people in this position are ‘food and nutrition service director’, ‘clinical dietitian’, ‘chef’ or ‘purchasing manager’.
-
5. ‘Sustainability’ is broadly defined as the use and distribution of goods, services and resources in a manner that does not deplete them, as compared with ‘environmental sustainability’ which specifically refers to natural resources (both renewable and non-renewable) and impacts overall civilization sustainability( Reference Goodland 23 ).
Evaluation aims
Nationwide, over fifty-two hospitals have signed the BMC yet few data exist on whether the strategies and tools provided by HCWH are being utilized or if hospitals are achieving the 20 % reduction in meat purchases( 20 ). Hospitals in the Maryland/Washington, DC region are leaders in the health-care industry and are also focused on improving the food environment. Many have adopted sustainable food policies; twenty-two hospitals in the region have signed the Healthy Food Pledge and twelve have signed the BMC( 20 ). To date, no evaluation of the BMC has been conducted in the Maryland/Washington, DC region.
Therefore we conducted a mixed-methods, retrospective assessment of hospitals in the Maryland/Washington, DC area that had adopted the BMC. The objectives were to assess (i) utilization of the toolkit and (ii) achievement of the 20 % reduction in meat purchases. The meat reduction strategies and each hospital’s experience with implementation were also summarized.
Experimental methods
Each hospital that signed the BMC was provided with an ‘implementation toolkit’ to facilitate implementation of the meat reduction strategies. The toolkit contained six tools that cover a variety of food service areas including tracking purchases, developing recipes, education and marketing. Strategies to reduce meat purchases were available online to each hospital that signed the BMC and in the toolkit. The strategies included reducing meat portion sizes, increasing vegetarian options and substituting cheaper cuts of meat; a complete list is provided in Table 2.
Table 2 Toolkit items and meat reduction strategies of the Balanced Menus Challenge
Participants
Hospitals were eligible for inclusion if they were located in the Maryland/Washington, DC region and signed the BMC. Initial contact was made to the food service director via email sent two months prior to conducting the survey. The email contained a welcome letter which introduced the project, purpose and scope, and requested a response from hospitals willing to participate.
Second contact was also made via email one month after the initial contact. Responders were asked for schedule availability and provided with information about what they could expect during the interview.
To limit the potential for recall bias, a PDF was created with images of each of the tools from the toolkit along with some of the meat purchasing questions. This file was sent to each participant with the second contact and participants were asked to view the PDF before and during the interview. It was anticipated that this process would allow participants to gather data prior to the survey as well as remind them of the tools.
If no response was received to schedule the interview, a third contact was made by telephone one week after the second contact. Two attempts were made to reach non-responders by telephone in the event that responses to the initial email(s) were not received.
Previous surveys
Data on BMC toolkit utilization and the 20 % reduction in meat purchases were retrieved from two sources: (i) a review of existing data from previous surveys; and (ii) a newly developed survey, the Maryland Hospital Food survey (MHF).
Three previously unpublished surveys were reviewed to gather data for the present study. The previous surveys were developed by HCWH and conducted online with primarily closed-ended questions. Fifteen questions from all three previous surveys applied to the BMC evaluation.
Health Care Without Harm 2011 and 2013 national survey responses
National Healthy Food in Health Care (HFHC) surveys conducted by HCWH in 2011 and 2013 covered all areas of sustainability in health care including food. In each of these surveys four questions were asked about meat purchasing; no questions were asked about the toolkit for BMC (Table 3).
Table 3 Participants for all surveys related to the Balanced Menus Challenge
* Hospitals 5, 8, 9 and 10 did not participate in any survey.
† Healthy Food in Health Care internal survey 2011.
‡ Balanced Menus Challenge internal survey 2012.
§ Healthy Food in Health Care internal survey 2013.
|| Maryland Hospital Food survey 2013.
2012 Balanced Menus Challenge national survey responses
The third HCWH survey analysed for the present study was the 2012 national BMC survey. This survey had twenty-six questions covering utilization of the toolkit, implementation of the strategies and assessment of the outcome goal of 20 % meat reduction. Three hospitals in our sample completed the national BMC survey. A total of six questions in this survey pertained to the objectives for our study.
Development of the Maryland Hospital Food survey
In addition to reviewing previous surveys, we developed and administered a twenty-question semi-structured interview: the MHF. It was divided into two sections to address each of the project objectives: Part 1 was designed to learn about toolkit utilization and motivation, while Part 2 asked for exact numbers of meat purchases, strategies for reducing purchases and route/source of meat procurement.
This survey used a combination of closed- and open-ended questions. Toolkit questions asked if hospitals received a specific tool and then if they used it. Two questions were open-ended to allow the respondent the opportunity to discuss their experience with the tools.
The questionnaire was reviewed and pre-tested by HCWH/Maryland Hospitals for a Healthy Environment (MD H2E) project coordinators. The study was reviewed by the Institutional Review Board of the University of Maryland School of Medicine and deemed non-human subject research.
Data analysis
Interviews were conducted and recorded by study staff by telephone using a free conference call number. After completing the interview, the responses were transcribed. The count, mean and mode of the closed-ended responses were calculated. The transcripts of the open-ended questions were compared for the mode response. Trends in meat purchasing were categorized into one of six categories based on the type of change made to the menu: ‘eliminated’, ‘reduced’, ‘substituted’, ‘increased’, ‘added’ or ‘substituted new source’. Pearson correlation statistics were calculated between BMC implementation toolkit receipt, toolkit use and implementation of BMC meat reduction strategies. Statistical analyses were performed using the statistical software package SAS version 9·4.
Results
Study sample
Twelve hospitals in the Maryland/Washington, DC region were identified as adopters of the BMC. One hospital was located in Washington, DC and eleven were located in Maryland.
Of the twelve hospitals, eight completed one or more of the four surveys and seven agreed to be interviewed for the MHF survey. All twelve hospitals were contacted at minimum twice and at maximum five times (mean=3·75) with an invitation to participate in the MHF survey. The MHF survey took an average of 27 min (range: 11–53 min) to complete. One of twelve hospitals participated in all of the surveys and another participated in three of the four surveys (Table 3).
The MHF survey had the highest response rate of all four surveys at 58 % (n 7). The final analysis was conducted with six hospitals because the survey revealed that the seventh hospital did not implement the BMC.
Non-responders
Five hospitals in the Maryland/Washington, DC region did not participate in the MHF survey. Two agreed to participate but were unable to complete the survey due to time constraints. One hospital changed food service management companies, which meant that none of the food service professionals who worked with BMC were available.
Previous survey results
The 2011 and 2013 HFHC surveys revealed that from 2010 to 2011, two hospitals reduced meat purchases: one reduced purchases by 18 % and adopted four strategies; the other reduced purchases by 5 % and adopted five strategies. From 2012 to 2013, two hospitals increased purchases of local and sustainable meat by an unspecified amount (Table 4).
Table 4 Results of the 2011 and 2013 Healthy Food in Health Care (HFHC) surveys
* For both HFHC national surveys, ‘animal-based protein’ refers to meat, poultry, seafood, dairy and eggs.
The strategies adopted were: increasing vegetarian options, switching meat-based meals to vegetarian, using meat as a condiment, switching to a more local source, reducing beef and pork, and increasing poultry.
The 2012 national BMC survey revealed that from 2010 to 2011, one hospital (two respondents) reported reductions in meat purchases that ranged from 20 to 30 %. They reported using three tools to accomplish the meat reduction: recipes, marketing materials and educational materials (Table 5).
Table 5 Results of the 2012 Balanced Menus Challenge internal survey by hospital (n 3)
N/A, not applicable.
Maryland Hospital Food survey results
Reducing meat purchases
Two hospitals reduced their meat purchases by ≥20 %. Meat purchase reductions were tracked either by the dollar amount or pounds of meat procured from local/sustainable sources. The purchases of local/sustainable meat among these two hospitals have increased since signing the BMC. One hospital reduced meat purchases, increased local/sustainable meat, and remained budget neutral two years after signing the BMC.
One hospital estimated that meat purchases reduced by 10 % but it did not track purchases; rather, it switched a portion of its budget (not specified) to more local and sustainable meat sources (Fig. 1). The remaining three hospitals did not quantify a reduction in meat purchases.
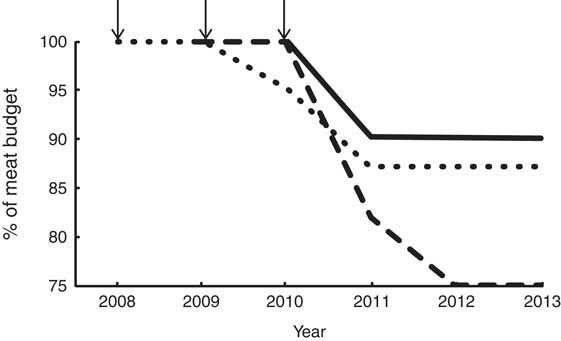
Fig. 1 Achievement of a 20 % reduction in meat procurement by hospital (![]() , hospital 1;
, hospital 1; ![]() , hospital 2*;
, hospital 2*; ![]() , hospital 12). *Hospital 2 results are the average from both respondents. ↓ indicates the year the Challenge was signed
, hospital 12). *Hospital 2 results are the average from both respondents. ↓ indicates the year the Challenge was signed
Toolkit utilization
The Balanced Menus brochure was received by all six of the participating hospitals. Marketing materials were received and used by four hospitals. The recipes were received and used by three hospitals. Educational materials were received and used by two hospitals. The greenhouse gas emissions tracking tool was received and used once by one hospital and the meat purchasing tracking tool was neither received nor used by any hospital (Fig. 2).
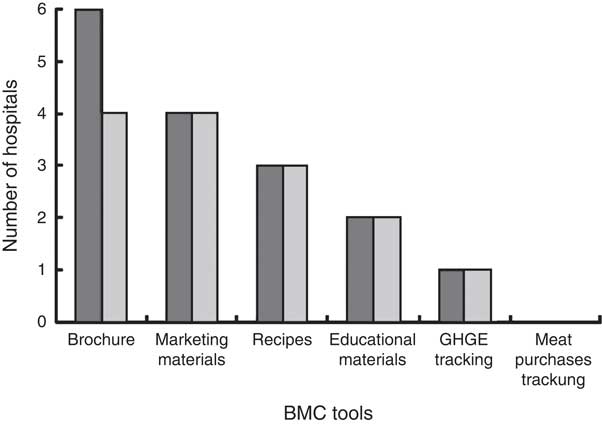
Fig. 2 Number of hospitals that received (![]() ) and used (
) and used (![]() ) the Balanced Menus Challenge (BMC) toolkit. GHGE, greenhouse gas emissions
) the Balanced Menus Challenge (BMC) toolkit. GHGE, greenhouse gas emissions
Meat reduction strategies
There were changes made in the cuts and variety of meats purchased and served at four of the six hospitals. One of the hospitals decreased the portion size of meat by 28·3 g (1 oz) for all meat menu items served. All four hospitals reduced or eliminated red meat (beef or pork) from the menu and three increased or substituted with poultry and fish. Three of four also increased vegetarian options or proteins (beans, legumes, soya protein, dairy protein). The most common strategy adopted was substituting one product with another (Table 6).
Table 6 Meat purchasing reduction strategies adopted by hospital (n 4)
Additional strategies to reduce meat purchases included: substituting ground turkey for beef, switching to local sources for fish and crab, substituting lunchmeat with a less processed source, increasing casseroles and reducing the number of times meat was served on the menu.
There was a positive correlation between receipt and usage of tools (r=0·93, P=0·005). However, there was no statistically significant correlation between receipt of tools and number of strategies implemented (r=0·37, P=0·47) or between usage of tools and number of strategies implemented (r=0·47, P=0·35; Fig. 3).
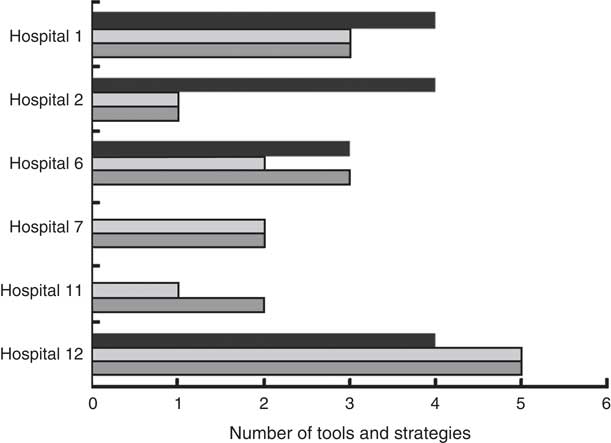
Fig. 3 Relationship between tool receipt (![]() ), tool use (
), tool use (![]() ) and meat reduction strategies implemented (
) and meat reduction strategies implemented (![]() ) by hospital
) by hospital
Source of meat procurement
The MHF survey asked if the route or source of meat procurement changed after signing the BMC. Since signing the BMC, one hospital purchased all meat and produce directly from local farmers. Two hospitals added meat and produce purchases from local and sustainable sources by an unspecified amount of the budget. The remaining participants indicated that they are under contract with a group purchasing organization or a contracted food service management company such that a minimum of 80 % of their purchases must be made through a designated supplier. The remaining 20 % of the budget is less restrictive and many of the hospitals indicated that this money may be available to make the changes to meat procurement.
Motivation for choosing the tools
Two questions were designed as open-ended responses to probe the motivations for choosing each tool from the toolkit. A common theme that emerged was that each hospital was interested in adopting healthy and sustainable food programmes, but there was push-back from patrons or a lack of administrative support to do so.
At the time of this survey, all of the hospitals were simultaneously implementing other healthy food programmes such as National Nutrition month, Meatless Mondays, the US Department of Agriculture’s Dietary Guidelines for Americans and the Heart Healthy Menu from the American Heart Association.
Respondents mentioned that the location of their hospital plays a role in their food sustainability choices. In addition, they noted that time, budget restrictions and contracts with food suppliers limit the changes they can make to procurement.
Discussion
The present evaluation shows that a sample of hospitals from the Maryland/Washington, DC area that participated in the BMC was able to reduce meat purchases and invest in local and sustainable meat after signing the Challenge. However, tracking purchases of sustainable meat was not prioritized. One hospital did demonstrate that switching to a local and sustainable source for meat is possible for at least a portion of the meal budget. None of the hospitals received all of the BMC tools despite the fact that they were available on the HCWH website. There was a significant correlation between the hospitals that received and used the highest number of BMC implementation tools; the same hospitals also adopted the most meat reduction strategies. However, it is important to emphasize that all of the hospitals were simultaneously implementing other healthy food programmes which could obfuscate the results of one programme.
Of the hospitals that reduced meat purchases, red meat (beef and pork) was reduced most often while poultry and vegetarian options simultaneously increased. Perhaps hospitals understood the message of the BMC and eliminated beef and pork from their menu because a sustainable option was not available. Two of the hospitals commented that this was the case. Conversely, a decrease in red meat only could be a misinterpretation of the terminology used in the BMC. Perhaps hospitals confused the term meat with red meat. In fact, some of the materials available to Challenge signers online use the phrase ‘meat and poultry’.
The present study also revealed that hospital food service professionals are personally committed to this food sustainability programme, but have limited autonomy to make changes. They have limited budgets, receive push-back from customers and are under contracts with group purchasing organizations. One hospital opted to change the menu to reduce meat but did not have the capacity to track purchases, so measuring the true impact was challenging. Reducing the amount of meat procured and served to hospital patrons is inherent in the design of the Challenge. However, any potential ethical considerations of purchasing and serving less meat per meal is something that a hospital may want to consider prior to accepting the Challenge. The BMC toolkit also contains marketing materials that allow a hospital to disclose to the patients and staff prior to the point of purchase about any changes that are made to the menu.
Inference on the correlation statistics is limited due to small sample size.
Despite the small sample size, the present study is a step towards addressing the need for outcome evaluations as suggested by the mounting evidence that most programmes like this go largely unevaluated( Reference Story, Kaphingst and Robinson-O’Brien 24 – Reference Larson, Story and Nelson 27 ). To date, no formal evaluation has been completed of the more than fifty-two BMC participants in the USA. In addition, the Challenge was adopted in 2011 by the Healthier Hospitals Initiative based on anecdotal evidence of success, such as the number of meat purchases reduced in pounds (lb); whereas the present study provides preliminary evidence of the impact of the Challenge( 28 ). The study also demonstrates that evaluation lags behind practice of institutional healthy food programmes to provide evidence for decision makers and stakeholders.
Future studies could opt for face-to-face interviews v. telephone interviews in order to achieve a higher response rate. However, little empirical evidence exists on the benefit, if any, of using one method over another in qualitative research( Reference Sturges and Hanrahan 29 , Reference Novick 30 ). Offering a financial incentive might also increase survey response rate as they have been shown to reduce non-response in telephone surveys( Reference Singer, Van Hoewyk and Maher 31 , Reference Kennet, Groerer and Bowman 32 ). This holds true for hospitals that are incentivized to collect and report quality data( Reference Lindenauer, Remus and Roman 33 ).
Finally, the present study is limited in generalizability due to regional differences between hospitals. Future efforts could also expand the sampling frame outside Maryland/Washington, DC to capture a larger number of BMC participants.
Acknowledgements
Acknowledgements: The authors thank Gina Navarro and Katherine Squibb PhD for their support in this work; also Lucia Sayre, Sapna Thottathil, Kathy Pryor, Colleen Funkhouser, MD H2E and HCWH for their contribution to developing the surveys and gathering hospital data. Financial support: C.L.M. and MD H2E received financial support from HCWH, the US Department of Agriculture Federal State Marketing Improvement Program, and the Jacob and Hilda Blaustein Foundation to provide support to hospitals on healthy meat purchasing initiatives in the Chesapeake region. The funders had no role in the design, analysis or writing of this article. Conflict of interest: The authors have no conflicts of interest to report. Authorship: T.D.R. developed and proposed the study for a Master’s Capstone experience, gathered all relevant data, conducted interviews and led the composition of the manuscript. C.L.M. and C.R.D. served as co-mentors of the project, contributed to the composition of the manuscript and reviewed drafts. C.R.D. performed the statistical analyses. D.M.S.G. served as Capstone director, contributed to the composition of the manuscript, reviewed drafts and served as the Principal Investigator for the University of Maryland Institutional Review Board application. Ethics of human subject participation: The MHF survey was approved by the Institutional Review Board of the University of Maryland School of Medicine as non-human subject research (HP-00056100 06/17/2013).














