Infant feeding practices such as breast-feeding and the timing of solid food introduction have significant health implications for both infants and mothers. Breast-feeding during the early months of an infant’s life has been linked to reduced risks of ear, respiratory and gastrointestinal tract infections, as well as sudden infant death syndrome( 1 ). For mothers, breast-feeding can decrease postpartum blood loss, facilitate transformation of the uterus after birth and reduce the risk of breast and ovarian cancers later in life( 1 ). Conversely, early introduction of solid foods has been associated with an increased risk for gastrointestinal infections( Reference Duijts, Jaddoe and Hofman 2 ) and chronic diseases (e.g. obesity), particularly among infants who received solids prior to 4 months of age( Reference Pearce, Taylor and Langley-Evans 3 ) and were breast-fed for a reduced period (or not at all)( Reference Grummer-Strawn, Scanlon and Fein 4 ).
Current WHO recommendations state that infants should be exclusively breast-fed for their first 6 months with continued breast-feeding, along with complementary food, for the first 2 years or more( 5 ). Other clinical recommendations, such as those from the American Academy of Pediatrics, suggest continued breast-feeding for at least the first year( 1 ). Furthermore, experts recommend not introducing solid foods until infants are at least 4 months of age( 1 ), with many recommending waiting until at least 6 months( 6 ). Developmentally, younger infants are not ready for solids because they still have the tongue-thrust reflex, cannot sit or hold their heads steady and cannot chew or control the movement of food around their mouths. Adding cereal to an infant’s bottle is specifically discouraged by the American Academy of Pediatrics as it may lead to overfeeding and excessive infant weight gain( Reference Shelov and Hannemann 7 ) and because there is no scientific support that adding cereal to milk can improve infant sleep( Reference Macknin, Medendorp and Maier 8 , Reference Rosen 9 ). Because infant feeding practices have long-lasting implications for childhood and even adult health( Reference Owen, Martin and Whincup 10 , Reference Parikh, Hwang and Ingelsson 11 ), it is important to understand the factors that shape feeding practices to inform public health interventions.
The rate at which mothers initiate breast-feeding in the USA, where the present study took place, has increased dramatically from 22 % in 1972( Reference Eckhardt and Hendershot 12 ) to 79 % in 2011( 13 ). However, the duration of exclusive breast-feeding falls short of clinical recommendations with only 18·8 % of US mothers reporting exclusive breast-feeding to 6 months in 2011( 13 ). In a large US sample, 40·4 % of mothers reported introducing solids (i.e. anything besides breast milk or infant formula) before the age of 4 months( Reference Clayton, Li and Perrine 14 ). Generally, little research has studied the practice of adding cereal to infants’ bottles compared with breast-feeding and factors that explain this behaviour are not well understood. One study available in the literature reported that most Hispanic mothers recognized that solid foods should be introduced at or about 4–6 months of infant’s age; however, many view adding cereal to bottles as an exception to this rule( Reference Woo Baidal, Criss and Goldman 15 ).
Despite the remarkable improvement in breast-feeding initiation rates in the USA over the last 40 years, a disparity continues to persist with mothers from low socio-economic backgrounds having a much lower initiation rate than their counterparts from high socio-economic backgrounds: 57 % and 74 %, respectively( Reference McDowell, Wang and Kennedy-Stephenson 16 ). Racial and ethnic differences in the early provision of solids have also been documented, where Black and Hispanic mothers are more likely to introduce solids before their infant is 4 months of age compared with White mothers( Reference Taveras, Gillman and Kleinman 17 , Reference Crocetti, Dudas and Krugman 18 ). In a sample of low-income African-American mothers, over 75 % of infants received juice or solids by 3 months of age( Reference Thompson and Bentley 19 ). One recent study reported cultural beliefs among Hispanic mothers that infants feel fuller, gain more weight, have better nutrition and are calmer and sleep longer when cereals are added to their bottles( Reference Woo Baidal, Criss and Goldman 15 ). Younger maternal age and lower educational attainment have also been associated with early introduction of solids( Reference Schiess, Grote and Scaglioni 20 – Reference Rebhan, Kohlhuber and Schwegler 22 ). Considering the lifelong health benefits of optimal infant feeding practices( 1 , Reference Pearce, Taylor and Langley-Evans 3 ), addressing the disparities in these infant feeding practices among mothers of low-income groups by understanding the factors that influence their feeding behaviours has the potential to address larger health disparity issues in the US population.
Research on infant feeding practices has focused primarily on such modifiable factors as feeding knowledge, intention, self-efficacy and the social support mothers receive related to various feeding methods( Reference Meedya, Fahy and Kable 23 ). Thus, many of the interventions on breast-feeding( Reference Maycock, Binns and Dhaliwal 24 – Reference Chung, Raman and Trikalinos 26 ) and early complementary feeding( Reference Black, Siegel and Abel 27 ) have focused on providing education to increase knowledge among mothers and their social support providers (e.g. spouse, own mother, health professionals). Focusing on the roles of social relationships to facilitate optimal infant feeding practices is based implicitly on the theory that members of a mother’s social environment (i.e. social network members or alters) can influence her own health behaviours( Reference Centola 28 – Reference Christakis and Fowler 30 ). Social influence can occur directly through the form of advice provision or indirectly through the form of internalized social norms( Reference Lewis and Rook 31 ). Numerous studies have shown the importance of subjective norms, or a mother’s evaluation of the degree to which important persons in her life endorse breast-feeding, and the perceived importance to comply with these individuals( Reference Swanson and Power 32 , Reference Avery, Duckett and Dodgson 33 ). Studies have also shown how social network members (e.g. spouses, grandmothers) armed with pro-breast-feeding knowledge can facilitate the extent to which mothers perceive their social environments as being supportive of breast-feeding( Reference Ingram and Johnson 34 – Reference Ma and Magnus 36 ).
Overall, researchers have spent a great deal of effort documenting whether network members with desirable health knowledge can facilitate recommended infant feeding behaviours, yet little attention has been paid to whether advice that goes against feeding recommendations can undermine a mother’s likelihood of engaging in recommended feeding behaviours. In short, does ‘bad’ advice hurt as much as ‘good’ advice can help? It would be incorrect to simply assume that such effects are naturally symmetrical. For example, imagine a mother who has a good friend who promotes exclusive breast-feeding and a good friend who promotes exclusive formula-feeding. How does the combined social environment affect the mother’s initiating of breast-feeding? Will the presence of undermining advice cancel out the presence of supportive advice? Or perhaps it is mainly the presence of supportive advice that matters. These empirical questions are the focus of our study. Exploring the symmetry of these effects has important implications for the development of interventions. Although much of the public health efforts to facilitate optimal infant feeding focus on enhancing positive support( Reference Renfrew, McCormick and Wade 37 ), it may well be that minimizing undermining social influence is equally or more important in developing optimal social contexts to support infant feeding.
To this end, the point of departure for the present study is that a mother’s social environment may be complex in terms of the advice she receives regarding infant feeding. Previous research indeed documents that mothers are often exposed to a mixture of advice, some of which is consistent with clinically recommended practices (e.g. to breast-feed) and some of which is clearly not aligned with official recommendations (e.g. to add cereal in bottle) during the first year of an infant’s life( Reference Woo Baidal, Criss and Goldman 15 , Reference Bentley, Gavin and Black 38 , Reference Heinig, Ishii and Banuelos 39 ). In a qualitative study, Hispanic mothers identified female family members as common sources of advice and examples of feeding routines, including practices that are counter to clinical guidelines such as adding cereal in infants’ bottles( Reference Woo Baidal, Criss and Goldman 15 ).
Thus, in order to advance our understanding of the complex social contexts that surround infant feeding behaviours, we (i) explicitly accounted for the (co)presence of supportive and undermining advice regarding feeding related behaviours and then (ii) investigated their respective associations with feeding outcomes (i.e. breast-feeding initiation, adding cereal to bottles). The key empirical question is whether social network members – i.e. their attitudes and beliefs that are passed on to mothers – can in fact hurt as much as they can help in facilitating optimal infant feeding practices. The analysis also distinguished between the effects of general health advice (i.e. all advice related to infant feeding practice) and advice related to specific behaviours (i.e. supportive and undermining advice associated with breast-feeding v. the introduction of solid foods specifically). Understanding these associations can shed light on whether public health efforts should focus on enhancing social influences supportive of optimal feeding practices or reducing influences that may undermine such behaviours, as well as whether specific forms of advice should be targeted in interventions.
Methods
Procedures
This was a cross-sectional survey study that involved interviews with mothers of infants between 0 and 12 months old about their social support networks in providing care to the infant. Each participating mother (ego) answered questions about her infant feeding behaviours and associated beliefs and attitudes. She was also asked to categorize her relationship with each social support network member (alter; e.g. family, friend, health professional) and to provide background information about herself as well as her support network members.
Eligible participants included those who were at least 18 years old, could converse in English and had a child who was less than 1 year old. Participants were recruited in-person and with flyers through the government-funded Women, Infants, and Children (WIC) clinics and a hospital-based out-patient general paediatric clinic primarily serving low-income children in an urban south-eastern city in the USA between September 2011 and June 2012. Mothers with a child less than 1 year old were identified by clinic staff during a routine doctor or WIC visit and subsequently introduced to interviewers who explained the study and enrolled those who were interested in participating. Respondents provided verbal consent prior to participating in the one-time interview. Interviews lasted between 20 and 45 min and each respondent received a $US 20·00 gift card to a retail store. A total of eighty-one mothers participated. Six interviewers were trained through a 4 h didactic session and a minimum of three mock interviews per interviewer with the principal investigators and research staff. There were no differences in key variables between the interviewers and adding dummy variables indicating interviewers did not affect our substantive results.
Measures
Infant feeding behaviours
The outcomes examined were two infant feeding behaviours considered beneficial according to clinical recommendations: (i) ever breast-fed (or initiation); and (ii) not adding cereal to the infant’s bottle. The ‘ever breast-fed’ outcome was determined by the response of ‘yes’ to the question: ‘Did you ever breast-feed your baby or feed him/her your pumped milk?’ The indicator of ever breast-fed was used because of the documented importance of any duration of breast-feeding on the well-being of infants and recent public health efforts to increase the uptake of breast-feeding( Reference Renfrew, McCormick and Wade 37 , 40 ). This set of analyses considered information obtained from eighty mothers (one person was excluded due to missing data). Second, participants were considered to exhibit desirable solid food behaviour (not adding cereal) if they answered ‘never’ to the question: ‘How often have you added baby cereal to your baby’s bottle of formula or pumped (or expressed) breast milk?’ US national data show that infants as young as 3 weeks receive cereal in the bottle( 41 ). This second set of analyses included fifty-five mothers with infants 21 d or older who had ever used a bottle to feed, excluding those with infants younger than 21 d who may not have had an opportunity to introduce solids yet.
Social contexts
The social environment of each participant was assessed using a two-step name generator: ‘First, please list persons who have been important to you during the past year such as family, friends and health professionals’ and ‘Who else is important to you in your daily life, especially in caring for and feeding your baby?’ After identifying network members (alters), a series of name interpreter questions was used to assess whether the respondent received health advice from each member and the mother’s perceptions regarding the strength and empathetic nature of each relationship( Reference Marsden and Campbell 42 , Reference Marsden and Campbell 43 ). Alter-level information was aggregated per respondent to create three types of network characteristics described below: (i) advice that supports clinical recommendations; (ii) advice that undermines recommendations; and (iii) the perception of empathy within the social environment.
Presence of supportive and undermining advice
Based on the list of identified members, participants answered ten questions, five assessing the presence of supportive advice (e.g. ‘Who has told you that you should (exclusively breast-feed/NOT exclusively formula-feed your baby)?’) and five assessing undermining advice (e.g. ‘Who has told you that you should (put cereal in the baby’s bottle/NOT exclusively breast-feed your baby)?’; see Table 1 for a complete list of questions). The infant feeding recommendations published by the American Academy of Pediatrics( 1 ) were used to determine whether each behaviour was recommended (supportive) or discouraged (undermining). For each respondent (ego), summary measures were calculated by summing the total pieces of supportive (or undermining) advice reported within her network and dividing by the total number of members (i.e. pieces of advice per alter). For example, a person who named five alters and reported ten pieces of supportive information receives two pieces of supportive advice on average per alter. Per alter impact is used because the Akaike Information Criterion and Bayesian Information Criterion for our multivariate models are substantially better compared with the cumulative presence of information (e.g. the total pieces of good information reported). The same approach was used to calculate specific types of supportive and undermining advice with respect to each outcome, breast-feeding and not adding cereal in bottle (see Table 1: questions S1, S2, S5, U1, U2, U5 for breast-feeding, and S3, S4, U3, U4 for not adding cereal). Both supportive and undermining health advice can be present in a given social environment, either from the same or different network members. Additionally, a ‘netpositive’ summary measure was calculated for each respondent’s social environment (i.e. pieces of supportive information per alter minus pieces of undermining information per alter). A positive netpositive score indicates that there is relatively more supportive information than undermining information, whereas a negative score indicates that the undermining outweighs the supportive information in the respondent’s network.
Table 1 Presence of supportive and undermining advice (number of alters 291) among a sample (n 80) of low-income mothers of infants between 0 and 12 months old in a south-eastern US city, September 2011–2012
Empathy
Emotional closeness is considered a primary dimension underlying the strength of ties( Reference Marsden and Campbell 42 , Reference Granovetter 44 ). Closeness was measured vis-à-vis the perception of empathy: respondents selected network members who ‘understands what [the respondent is] going through’. The ‘proportion empathetic’ was calculated by dividing the number of network members selected as ‘understanding’ by the total number of alters elicited, with higher values corresponding to the respondent recollecting a more empathetic environment.
Covariates
Based on previous studies showing a strong association between mothers’ infant feeding belief and feeding behaviour, an indicator variable was created for respondents who answered that the best way to feed the baby is ‘formula feeding’( Reference Kaufman, Deenadayalan and Karpati 45 ). This variable was included as a covariate to assess the roles of social environment in explaining outcome variance above and beyond this particular belief. In addition, the demographic characteristics previously shown to be associated with infant feeding behaviours and also considered in the current study include: maternal age, infant’s age in days, race (African American), education (less than high school diploma)( Reference Chin, Myers and Magnus 46 ) and parity (multiparous)( Reference Li, Ogden and Ballew 47 , Reference Ryan, Wenjun and Acosta 48 ).
Analyses
A series of four logistic regression analyses was used to model each outcome (i.e. ever breast-feeding, adding cereal to bottle). In the first model, the outcome (yes/no) was modelled as a function of background characteristics (i.e. education, race). Participant’s belief that formula is the best way to feed was also included as a background characteristic in the breast-feeding model. The second model for each outcome included two additional variables characterizing respondent’s self-reported social environment: empathy and netpositive. The third model decomposed the overall health information environment (netpositive) into the presence of supportive and undermining advice, allowing us to test their relative importance. Finally, the fourth model decomposed the health information environment even further by separating out pieces of supportive and undermining health advice that are specific to the behavioural outcome.
Results
Social environment of the participants
A total of 291 network members (alters) were identified by eighty mothers, with an average reported number of alters of 3·6 (sd=1·99, range=1–11). Approximately 8 % of those approached and given study information refused participation due to lack of time as mothers often needed to leave the clinic soon after their appointment was over. The average age of the participants was 24·6 years (sd=5·49), ranging from 18 to 40 years. As shown in Table 2, the majority was African American (80 %), had only one child (80 %) and did not believe that formula is the best way to feed the infant (90 %). Close to one-third (27 %) of the network members identified by the participants were their parents (the vast majority of whom, 85 %, corresponded to the respondent’s mother), 18 % of the network alters were spouse/partner or the infant’s father, 13 % were siblings, 9 % were friends and 6 % were health professionals. About one-third of these network members (32 %) were living with the participant at the time of the interview. Because age and parity were not significantly associated with either outcome (i.e. ever breast-feeding, adding cereal), they were not included in the further analysis.
Table 2 Participant (ego) characteristics among a sample (n 80) of low-income mothers of infants between 0 and 12 months old in a south-eastern US city, September 2011–2012
Participants reported the presence of both supportive and undermining information regarding infant feeding (Table 1). With respect to supportive advice, 22 % of the 291 alters had advised respondents to ‘exclusively breast-feed’ and 41 % had advised respondents to ‘NOT give solid foods’. In terms of undermining advice, participants reported receiving advice to ‘put cereal in the baby’s bottle’ and ‘exclusively formula-feed’ from 31 % and 13 % of alters, respectively.
Table 3 presents a summary of the network characteristics. Respondents, on average, reported the presence of one piece of information supportive of clinical recommendations per alter (mean=1·1, sd=1·1, range=0–4·5) and 0·8 piece of undermining information per alter (mean=0·8, sd=0·8, range=0–3·0). In terms of the information specifically about solid food, the average per alter measures were 0·6 (mean=0·6, sd=0·6, range=0–2·0) and 0·3 (mean=0·3, sd=0·5, range=0–2·0) for supportive and undermining advice, respectively. For breast-feeding, the average per alter measures were 0·5 (mean=0·5, sd=0·6, range=0–2·5) and 0·4 (mean=0·4, sd=0·6, range=0–2·7) for supportive and undermining advice, respectively. There was substantial variation in terms of the amount of empathy reported in networks (range=0–1); on average, respondents indicated that about half of their network alters ‘understood them’ (mean=0·5, sd=0·3). The average netpositive was 0·3 (sd=1·4), indicating a fairly neutral overall social environment in terms of the presence of supportive and undermining information. However, the measure ranged between −2·7 and 4·5 suggesting that some participants reported predominantly undermining where as others reported supportive environments.
Table 3 Characteristics of participants’ infant feeding support networks among a sample (n 80) of low-income mothers of infants between 0 and 12 months old in a south-eastern US city, September 2011–2012
To better understand the composition of health information environments, participants were divided into four categories according to the presence of ‘pieces of information’ in the social environment: (i) low information (n 17; zero to one piece of information for each of supportive and undermining); (ii) primarily undermining (n 13; zero to one piece of supportive and two or more pieces of undermining information); (iii) mixed environment (n 29; two or more pieces of information of each type); and (iv) primarily supportive environment (n 21; two or more supportive and zero to one undermining). In the absence of prior research on health advice environments, our typology (low, primarily bad/good, mixed) corresponds to empirically relevant distinctions associated with our sample. Most participants reported mixed feeding-related information environments (36 %) followed by primarily supportive (27 %), low information (21 %) and primarily undermining (16 %). A higher proportion of mothers reporting primarily supportive environments reported ever breast-feeding (82 %) compared with those in primarily undermining information environments (46 %; see Fig. 1). A similar pattern held for never adding cereal. The type of information environment did not appear to be correlated with participants’ age, race/ethnicity or education level (see Table 4). Based on an F test for differences in group means, the average level of ‘empathy’ was mean=0·4 for the mixed environment group, which is statistically different (Scheffé multiple comparison test: P=0·04) from the level reported in the primarily supportive group (mean=0·7). The average age of the baby was younger (mean=49 d) for the primarily supportive environment group compared with the low information (mean=129·6 d, P=0·06), primarily undermining (mean=168 d, P<0·01) and mixed environment groups (mean=151 d, P<0·01).
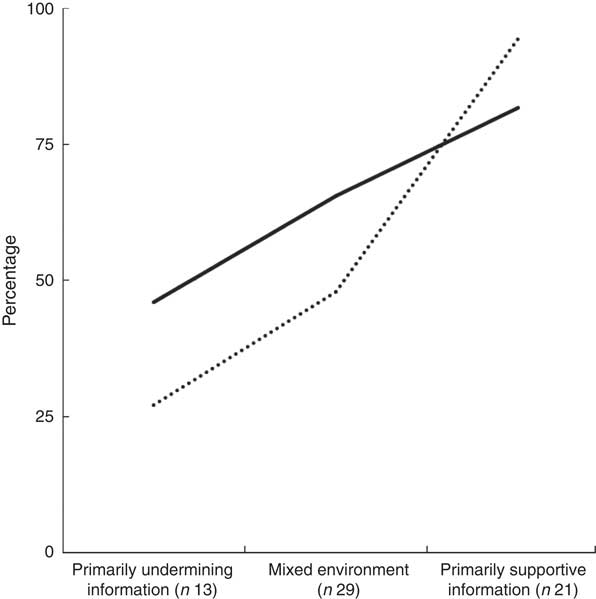
Fig. 1 Network effects on infant feeding behaviours: percentage who initiated breast-feeding (———) and percentage who never added cereal to the infant’s bottle (· · · · ·) by health information environments among a sample (n 80) of low-income mothers of infants between 0 and 12 months old in a south-eastern US city, September 2011–2012
Table 4 Respondent characteristics by health information environments among a sample (n 80) of low-income mothers of infants between 0 and 12 months old in a south-eastern US city, September 2011–2012
Social environment and infant feeding behaviours
Roughly 67 % of the eighty mothers reported ever breast-feeding, and 45 % of fifty-five mothers who had ever used a bottle and had infants 3 weeks or older reported not adding cereal to their infant’s bottle. Tables 5 and 6 present the logistic regression results for ever breast-feeding and not adding cereal to a bottle, respectively. The first model for breast-feeding presents the estimates of the likelihood of ever breast-feeding as a function of education (less than high school: OR=0·2; 95 % CI 0·1, 0·8) and the mother’s belief that formula-feeding is the best way to feed an infant (OR=0·1; 95 % CI 0·0, 0·8). Infant’s age was the only significant covariate associated with cereal-adding behaviour (OR=1·0; 95 % CI 1·0, 1·0). In the second model, the results suggest that mothers were more likely to comply with clinically recommended infant feeding behaviours when the supportive advice in their networks outweighed the undermining. Adjusting for the strengths of empathy, respondents who heard more supportive than undermining advice in general were more likely to have ever breast-fed; we expect mothers to be 1·8 times more likely to ever breast-feed (OR=1·8; 95 % CI 1·1, 3·0) for a one unit increase in netpositive. For example, consider two mothers who each report two pieces of undermining advice (per alter) and are otherwise the same on all other characteristics; the mother who reports three pieces of positive advice has 1·8 times the odds of initiating breast-feeding (on average) compared with the mother reporting only two pieces of positive advice. Having a relatively more supportive than undermining information environment was marginally associated with the cereal-adding behaviour (OR=1·8; 95 % CI 0·9, 3·7).
Table 5 Factors predicting breast-feeding initiation among a sample (n 80) of low-income mothers of infants between 0 and 12 months old in a south-eastern US city, September 2011–2012
AIC, Akaike Information Criterion; BIC, Bayesian Information Criterion.
*P<0·05.
† Refers to per network alter.
Table 6 Factors predicting not giving cereal in a bottle among a sample (n 55) of low-income mothers of infants between 0 and 12 months old in a south-eastern US city, September 2011–2012
AIC, Akaike Information Criterion; BIC, Bayesian Information Criterion.*P<0·05, **P<0·01, ***P<0·001.
† Refers to per network alter.
The third model decomposes the effect of netpositive into the effect of supportive v. undermining advice but it does not disentangle the topic of the advice (i.e. breast-feeding v. adding cereal). Model 3 shows that the presence of supportive information was significantly associated with the likelihood of ever breast-feeding (OR=2·0; 95 % CI 1·0, 3·8) and not adding cereal in the bottle (OR=2·3; 95 % CI 1·1, 5·0), whereas undermining information was not associated with these outcomes. Finally, model 4 decomposes supportive and undermining advice into specific types of advice. The results show that supportive information related to breast-feeding was significantly associated with ever breast-feeding (OR=6·7; 95 % CI 1·2, 38·1) as well as not adding cereal (OR=15·9; 95 % CI 1·1, 227·4). However, undermining information about breast-feeding and information about solid foods were not associated with either outcome. Thus, it appears that the effects of netpositive on breast-feeding behaviour (observed in the second model) can be explained primarily by the positive role of supportive breast-feeding advice. Similarly, the effect of general supportive advice in model 3 for cereal behaviour (Table 6) can be attributed to the positive role of supportive breast-feeding behaviour.
The model fit statistics for both behaviours improved significantly in the second, third and fourth model compared with the first model, suggesting the importance of the social network factors in understanding infant feeding behaviours. As expected, the fit of the model did not improve from the second to the fourth model as these three models were used to decompose the overall effect of netpositive (model 2) into the specific effects of supportive v. undermining information (models 3 and 4). Finally, when comparing the effect of network empathy to the effect of the information environment (e.g. netpositive), the results suggest overall that the composition of health advice was more strongly associated with infant feeding behaviours than the presence of empathetic alters.
Discussion
The present study evaluated the presence of health information regarding infant feeding, specifically the impact of advice that supports v. undermines clinical recommendations, and how such social contextual factors are associated with two types of infant feeding behaviours, ever breast-feeding and adding cereal to the infant’s bottle. Findings indicate that both types of infant feeding advice (supportive and undermining) are present at high frequency within mothers’ social support networks and that self-reported characteristics of these social networks (i.e. the composition of health advice) significantly improves our understanding of mothers’ infant feeding behaviours. The presence of feeding information supporting clinical recommendations appears to be associated with both behaviours explored in the study, ever breast-feeding and not adding cereals. Namely, the presence of information specifically supportive of breast-feeding was significantly associated not only with ‘ever breast-feeding’ but also with never adding cereals in the bottle. What this suggests is that the cultural norms around breast-feeding may be ‘stronger’ than the cultural norms around the introduction of solid foods in mothers’ social environments. Thus, the social norm to breast-feed infants may have stronger implications on mothers’ perceptions and behaviours than the social norm to not introduce solids early.
Using two elicitation questions, participants enumerated roughly three-and-a-half social network members (alters) whom they likely associated with infant care and feeding. Although the first elicitation question sought to elicit participants’ general social support system, the way the current study was presented to the participants at the time of the recruitment (a study about infant feeding) may have led participants to enumerate a specific subset of the overall support network system that is involved in infant care. The majority of the network members (66 %) listed by the participants were relatives including parents, siblings, aunts/uncles, grandparents and cousins. Eighteen per cent were participants’ spouse/partner or the infant’s father and 6 % were health-care professionals. Thus, as speculated in previous studies( Reference Maycock, Binns and Dhaliwal 24 , Reference Pisacane, Continisio and Aldinucci 35 ), these data validate the effort to influence social norms about infant feeding vis-à-vis family and relatives.
Most participants reported being in mixed message environments regarding infant feeding. That is, respondents simultaneously receive – from various members or even from the same member – advice that supports and undermines clinical recommendations. Only 16 % of the participants reported low information environments (one or fewer pieces of supportive and undermining advice each) whereas 84 % reported the presence of at least two pieces of advice for either or both types of information. Mothers of younger infants tended to report more supportive than undermining or mixed environment. At the alter level, a large proportion (41 %) of the 291 support network members identified by the participants had told the mother that they ‘should NOT give solid foods’ to the infant before 4 months of age and about one-fifth told the participants to ‘exclusively breast-feed’, supporting clinical recommendations. On the other hand, about one-third of the network members told the mothers to ‘put cereal in the baby’s bottle’ and 13 % said that they ‘should exclusively formula-feed’, undermining clinical recommendations. Our findings augment previous studies of infant feeding advice( Reference Woo Baidal, Criss and Goldman 15 , Reference Bentley, Gavin and Black 38 ) by highlighting that such advice is passed through networks at a very high frequency and that mothers tend to receive mixed messages.
Mothers who reported hearing more overall supportive compared with undermining information (netpositive) were more likely to have ever breast-fed; this measure was also marginally associated with never adding cereal to the infant’s bottle. Further analyses, however, showed that when this netpositive measure is ultimately decomposed into specific types of supportive and undermining advice, the presence of supportive advice specifically about breast-feeding was the only factor associated with ever breast-feeding as well as not adding cereal in the bottle. It may be that mothers who received information supportive of breast-feeding were more likely to breast-feed and, as studies have shown, breast-feeding mothers are less likely to introduce solids before 4 months compared with mothers who formula-feed or mix-feed their infants( Reference Clayton, Li and Perrine 14 ). Altogether, our results suggest that optimal infant feeding behaviours may be facilitated by focusing on increasing supportive advice related to breast-feeding while concentrating less on reducing either form of undermining advice (i.e. add cereal, do not exclusively breast-feed) within mothers’ networks.
Public health interventions to facilitate optimal infant feeding practices have focused on the provision of information supportive of desired feeding practices from health professionals( Reference Meedya, Fahy and Kable 23 , Reference Merewood and Heinig 49 , Reference Wen, Baur and Simpson 50 ). Our findings suggest the importance of such information that originates from mothers’ close social support network members such as relatives and friends. Interventions to facilitate optimal infant feeding need to involve mothers’ support network members so that the types of advice provided to them can be targeted for change. Interventions that involved mothers’ partners and parents have shown success in increasing breast-feeding initiation and maintenance( Reference Ingram and Johnson 34 – Reference Ma and Magnus 36 ). The data from the current study elucidate other potentially important network members such as extended family and relatives (e.g. siblings, aunts/uncles, cousins). Identifying network members who play key roles in providing feeding advice to mothers by means of the social network assessment methods used herein may be useful in order for the interventions to reach beyond predetermined family members such as partners and mothers.
The current study also elucidates the complex nature of the social environment surrounding mothers feeding their infants. More studies are needed to understand how complex social environments (e.g. mixed information environment) influence infant feeding behaviours among mothers. It may be that the presence of supportive information about breast-feeding serves as a proxy for overall knowledge about infant feeding recommendations. Due to a heavy emphasis on breast-feeding in infant feeding education programmes( Reference Meedya, Fahy and Kable 23 , 51 ), it may be that education about solid foods that tends to come from paediatricians may not be reaching the mothers in a timely manner; for example, before they consider adding cereal in the bottle. Our findings indicate that the presence of information about one behaviour, breast-feeding, was also associated with another behaviour, not adding cereal. This suggests that providing information regarding these two behaviours together in health education programmes for expecting and new mothers may be beneficial. Future research and interventions may consider the potential implications of health information about a specific behaviour (e.g. breast-feeding) on other behaviours (e.g. early introduction of solid foods, feeding to calm/reduce infant distress rather than in response to hunger cues), to understand unintended effects that can be both positive and negative. Such knowledge can inform how practitioners can link the information regarding different feeding practices together as such information is likely to interact with each other to influence feeding behaviour outcomes. A comprehensive understanding of the constellation of information and advice in a mother’s social network is needed to achieve overall desirable feeding behaviours and health outcomes.
In the present study, efforts were made to interview participants from a hard-to-reach and under-studied population. As a result, the majority of the participants were of ethnic minority background from a low-income, urban area in the south-eastern USA. Therefore, the study findings may not be generalized to others who have different cultural and social backgrounds. Participants’ social contexts were evaluated through self-report by assessing their ego-centred network systems. The characteristics of social relationships reported by the participants were not verified by others in their networks. The interpretation of ‘low information’ environment is a little unclear as it could represent the environment in which health advice is relatively absent or alternatively could mean that respondents chose not to report health advice (i.e. a missing data problem potentially due to such biases as recall and social desirability). The study was cross-sectional, involving a small sample of mothers. Our results cannot demonstrate whether the presence of information has a causal effect on mothers’ behaviours (i.e. cannot tease apart whether the results are due to information impacting behaviour, contagion, or those with similar attitudes and behaviours interacting with each other more, homophily). Participants were also young and similar in age, with the vast majority (80 %) falling between the ages of 18 and 28 years (median=23 years, mode=20 years). This may have led to the observed non-significance in its association with the infant feeding behaviours. The sample size for the analyses concerning cereal-adding behaviour was particularly small, likely limiting our ability to identify key factors associated with feeding behaviours. Future studies should be conducted using a longitudinal design with a larger sample of mothers so that the roles of their social contexts preceding behavioural occurrences can be examined.
It is worth noting that these findings cast serious doubt on the assumption of symmetry with respect to social influence and health behaviours. For example, a friend suggesting to another friend that exercise is beneficial is promoting a behaviour that is already broadly endorsed by health experts at large, in which case such advice dovetails with generalized beliefs around optimal health behaviours (e.g. ‘I already know that I should be exercising and now my friend has reminded me’). In contrast, a friend who encourages another to smoke is giving advice that counters generalized beliefs. In order for this advice to be impactful, the ego would have to be persuaded to go ‘against the tide’. As the present study findings suggest, and is also seen in current infant feeding education programmes( Reference Meedya, Fahy and Kable 23 , 51 ), the culture surrounding breast-feeding may be stronger than the culture surrounding introduction of solid foods in our society. It is likely that mothers would have to work harder to go against the social tide of breast-feeding than not adding cereal. Therefore, public health efforts to discourage adding cereal to bottles targeted to the general public may be beneficial in creating a social tide that not only influences mothers’ knowledge but also the social influence processes within mothers’ personal web of social relationships. Future research should consider measuring the presence of both supportive and undermining advice regarding various infant feeding behaviours within mothers’ social contexts, and evaluate the extent to which such information (co)exists or interacts to influence infant feeding outcomes.
Acknowledgements
Acknowledgement: The authors would like to thank their interviewers and the mothers who participated in the study. Financial support: This study was funded by the Center for Health Equity Research at the University of Memphis School of Public Health awarded to S.A. and N.A.W. The Center for Health Equity Research at the University of Memphis School of Public Health had no role in the design, analysis or writing of this article. Conflict of interest: None. Authorship: S.A. formulated the research question, designed and carried out the study and wrote the article. F.B.L. formulated the research question, analysed the data and wrote the article. N.A.W. designed and carried out the study and assisted in writing the article. E.J.S. carried out the study and assisted in writing the article. Ethics of human subject participation: This study was conducted according to the guidelines laid down in the Declaration of Helsinki and all procedures involving human subjects were approved by the Institutional Review Board of the University of Memphis and University of Tennessee Health Science Center. Verbal informed consent was obtained from all participants. Verbal consent was witnessed and formally recorded.












